선천성 식도폐쇄에서 발생한 선천성 기관연화
한석주, 정은주, 김세헌1, 윤춘식2, 심규대3, 남용택3, 김재억4, 황의호
연세대학교
외과학교실, 이비인후과교실1, 진단방사선과학교실2, 마취과학교실3
및 소화아동병원 소아외과4
서 론 선천성 기관연화(tracheomalacia)는 기관연골의 선천성 약화로 인하여 기관폐쇄를 일으키는 질환으로 선천성 식도폐쇄(esophageal atresia)와 연관되어 자주 발생하는 것으로 알려져 있다. 선천성 기관연화에 대해서는 소아외과 교과서에 잘 기술되어 있으며,1-5 이를 근거로 하여 추측하여 보면 선천성성 식도폐쇄를 다루게 되는 국내 소아외과 의사들 역시 기관연화를 드물지 않게 만났을 것으로 생각된다. 그러나 본 연구자가 확인한 바로는 선천성 식도폐쇄와 관련하여 발생한 선천성 기관연화에 대한 국내보고는 찾아 볼 수 없었다. 본 연구자는 그 동안 선천성 기관연화를 치료함에 있어 여러 어려움이 있어 온 것이 사실이다. 그 이유는 본 연구자를 포함하여 국내에서는 아직 이 병에 대한 경험과 인식 부족, 그리고 이로 인한 두려움이 있어 왔던 것이 사실이기 때문이다. 이에 본 연구자는 최근 경험한 선천성 식도폐쇄와 동반되어 발생한 전형적인 기관연화를 보고하면서 기관연화에 대하여 논하여 보고자 한다.
|
|
|
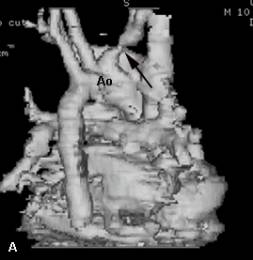
Fig. 1. The esophagography
is showing no stricture of the esophageal anastomosis and recurrent
tracheoesophageal fistula. Note the tracheal air shadow. The tracheal air
shadow disappears in a region (black arrows) as the tracheal collapse during
expiration. |
증 례 11개월 남아가 7개월 전부터 시작된 간헐적인 수유 도중의 급성 호흡곤란과 청색증의 원인을 찾기 위하여 타 병원에서 식도조영술을 시행 중 호흡곤란이 발생하여 심폐소생술로 소생된 후 전원되었다. 환아는 재태기간 38주에 출생체중 2900gram으로 제왕절개술로 태어났으며 생후 제 2일에 선천성 식도폐쇄(Gross type C)로 교정수술(total correction)을 받고 식도문합부협착이 있어 수 차례 식도확장술을 시행 받았다. 전원당시 청진상 호기 협착음(expiratory stridor)과 우측 흉부에 수술흉터 외에 이학적 검사상 다른 이상 소견은 없었다 입원 후 시행한 식도조영술에서 협착부나 기관식도루는 관찰되지 않았으나 문합부 인접 기관의 내경이 호기(expiration) 시 좁아지는 현상이 관찰되었다
(그림 1).
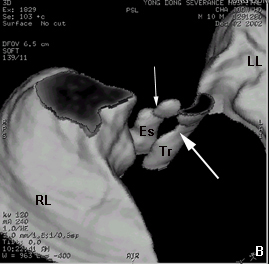
24시간 식도 pH측정 검사(24 hours esophageal pH monitoring)에서 역류지수(reflux index)가 4%로 의미 있는 위식도역류(gastroesophageal reflux)는 없는 것으로 판단되었다. 심초음파 소견은 정상이었다. 흉부 컴퓨터단층촬영의 3차원 구성(three dimensional reconstruction of chest CT)에서 대혈관의 기형은 관찰되지 않았으나 무명동맥 기시부(origin of innominate artery)가 함몰된 소견을 보이면서 인접부위로 추측되는 기관의 함몰소견이 동시에 관찰되었다(그림 2).
|
|
|
|
||
|
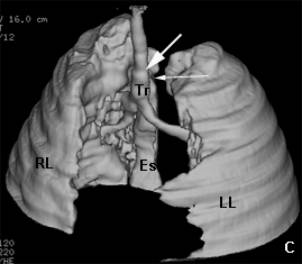
Fig. 2. (A) The
left posterior oblique view of great vessels and heart in preoperative 3-D
reconstruction of chest CT scan is showing an indentation (black arrow) of
the innominate artery that was made by compression of the trachea. (B) The
superior right anterior view of trachea, esophagus and lung in preoperative
3-D reconstruction of chest CT scan is showing a depression (white large arrow)
of the trachea that would be made by innominate artery and the esophageal
anastomosis site (white small arrow). (C) The left anterior oblique view of
trachea, esophagus and lung in postoperative 3-D reconstruction of chest CT
scan is showing no depression (white large arrow) of the trachea but showing
the persistent existence of the esophageal anastomosis site (white small
arrow). Abbreviations: Ao; aortic arch, RL; right lung, LL; left lung, Es; esophagus, Tr; trachea
|
||||
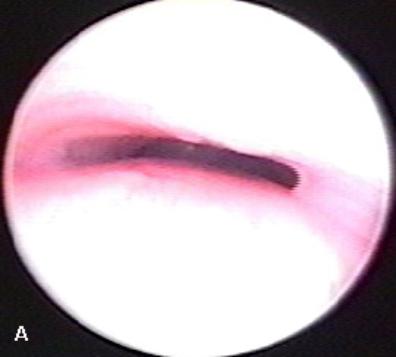
자발 호흡이 있는 전신마취 상태에서 시행한 강성 기관지경(rigid bronchoscopy) 검사상 기관분지(carina)로부터 약 1.5cm 상방에서 호기 시 전후 직경이 감소하는 심한 기관함몰이 관찰되어서 기관연화를 확진 할 수 있었다(그림 3-A). 환아는 입원 11일간 발생 한 적이 없는 질식 소발작(apneic spell)이 기관지경 검사 직후 발생하더니 계속 반복하여 중환자실로 전실 되었다. 기관연화로 인한 질식 소발작의 최종진단 하에 기관지경 검사 후 제 2일(입원 제 13일)에 대동맥고정술(aortopexy)을 시행 받았다. 수술 중 기관지경을 동시에 시행하였으며 기관지경상 기관함몰이 대동맥고정술을 시행함으로써 소실됨을 확인하였다(그림 3-B).
|
|
|
|
|
Fig. 3. The bronchoscopic
view of the trachea in spontaneous breathing. (A) Before aortopexy, Note
elliptical narrowed lumen and bulging of elongated membranous trachea
posteriorly. (B) After aortopexy. The tracheal lumen is now wider during all
phase of respiration. |
||
|
|
|
|
환아는 수술 즉시 수술 전 들리던 호기 협착음은 더 이상 들리지 않게 되었다. 수술 후 제 6일에 흉부 컴퓨터단층촬영으로 추적한 결과 수술 전 보이던 기관의 함몰부위가 없어졌음이 확인되었다 (그림 3-C). 환아는 수술 제 9일(입원 제 22일)에 퇴원하여 환아는 현재 수술 후 5개월로 폐염이나 질식 소발작 없이 성장하고 있다.
고 찰 기관연화는 선천성 식도폐쇄와 자주 동반하는 질환으로 알려져 있다. 동반 빈도를 살펴보면 선천성 식도폐쇄 환자의 약 37%-68% 에서 동반된다고 하며,6, 7 심지어는 증세의 정도의 차이는 있으나 선천성 식도폐쇄 환자에서 모두 관찰되기도 한다고도 하니8 선천성 식도폐쇄의 치료에 중심이 되고 있는 소아외과 의사들에게는 이 병의 중요성을 강조하지 않을 수 없다. 본 연구자가 선천성 식도폐쇄를 수술하기 시작한 초기에 식도폐쇄 수술 후 별 문제 없이 퇴원하여 잘 자라던 환자가 수개월 후 갑자기 사망하였다는 소식을 접한 경험이 있다. 사망당시 상황과 이 환자에서 기관연화의 특징적인 물개 울음소리와 비슷한 기침 (seal bark cough)이 있었다는 점 그리고 다른 장기에는 갑작스러운 사망원인이 될 원인이 없었음을 종합하여 볼 때 선천성 식도폐쇄와 동반된 기관연화를 간과하여 생긴 질식 소발작(apneic spell)이 사망 원인이라고 생각한다. 그 후에도 선천성 식도폐쇄와 동반된 기관연화가 의심되는 환자를 치료하는데 있어서 경험부족과 지식의 부족으로 인하여 관련 타과에 환자를 의뢰하여 이를 해결하고자 하였었다. 그러나 관련 타과 역시 정확한 진단과 치료 방침을 내리지 못하고 환자는 결국 기관 절개술(tracheostomy)을 받고야 마는 것을 수 차례 보아왔다. 그 후 이 병에 대한 지식과 경험이 쌓이면서 이 질환은 타과에 의뢰할 질환이 아니고 소아외과 의사가 주축이 되어 다루어야 할 질환이라는 결론을 내리게 되었다. 아직 그 원인은 밝혀지지 않았지만 기관연화의 전형적인 증세는 대부분 생후 2-3개월까지는 보이지 않다가 그 후에 나타나게 된다.9 선천성 식도폐쇄를 다루는 소아외과 의사에게서는 기관연화에서 이러한 증세의 지연발현현상(delayed manifestation of symptoms)에 특히 주의를 요하여야 한다. 즉 선천성 식도폐쇄 환자가 퇴원하게 되면 보호자에게 기관연화의 증세를 환기시키고 외래에서 이를 주의 깊게 관찰하는 것이 중요하다. 거의 모든 기관연화에서는 정도의 차이는 있으나 취주악대의 금관악기 소리(brassy cough) 또는 물개울음 소리(seal bark) 등으로 표현되는 특징적인 기침소리나 울음소리를 들을 수 있다. 청진을 하면 호기 천명음을 청진할 수 있는 경우가 많다.1 이런 잡음은 호기 시 흉곽내압(intrathoracic pressure)이 증가하고 이로 인하여 약한 연골을 가진 기관내경이 좁아지게 되고 좁아진 부위를 빠져나가는 공기의 난류로 인하여 형성된다. 대분분의 환자는 위에서 언급한 특징적인 호흡 잡음 외에 다른 특별한 호흡기 증세를 나타내지 않는다. 기관연화는 1 세 이후에는 대부분 증세가 사라지는 것이 보통이다. 따라서 호흡 시 잡음만 들리며 심각한 합병증을 동반하지 않는 기관연화에서는 적극적인 진단과정이나 치료가 필요하지 않다.10 그러나 좀 더 심한 기관연화의 경우는 반복적인 폐염이 오게 되며 때로는 생명을 위협하는 질식 소발작이 오게 되는 경우가 있다. 이 경우는 기관 삽관(intubation) 혹은 심폐소생술이 필요하게 되기도 한다. 질식 소발작은 보통 수유 중이거나 수유를 마치고 5분에서 10분 이내에 발생하는 경향이 있으며 환자는 갑자기 축 늘어지면서 창백하여 지거나 파랗게 질리게 된다. 이 때 처치가 늦게 되면 사망하거나 영구적인 뇌 손상을 초래하게 된다. 수유와 질식 소발작 발생과의 관련성은 다음과 같이 설명되고 있다.9 수유 시 식도에 음식이 가득차게 되면 식도가 기관연화가 있는 부위의 기관막부(membranous portion of trachea)를 내측으로 밀게 된다. 이 때 기관의 내경이 좁아지게 되면 환자는 호흡 곤란을 느끼게 된다. 호흡곤란을 느끼고 당황한 환자는 좀 더 힘차게 호흡을 하려고 한다. 환자가 호기를 힘있게 하면 할수록 흉곽내 압력은 높아지고 기관의 폐쇄는 결국 더욱 심해지게 된다. 이런 상황에 빠지면 환자는 순간적으로 저산소증에 빠지면서 외부의 도움이 없으면 사망하게 되는 것이다. 이런 질식 소발작은 선천성 식도폐쇄 수술 후 발관(extubation) 직후에도 발생하는 경우가 있다. 따라서 선천성 식도폐쇄 수술 후 발관에 계속 실패하는 환자의 경우에는 기관연화의 동반 가능성을 한번은 생각하여 보아야 한다.
선천성 식도폐쇄와 연관된 기관연화의 진단을 함에 있어서 무엇보다 중요한 것은 비슷한 증세를 나타내는 다른 원인을 철저히 배제하는 것이다. 그 이유는 선천성 식도폐쇄의 수술 합병증이나 선천성 식도폐쇄와 연관되는 다른 질환이 아주 유사한 증세를 나타낼 수 있기 때문이다. 더군다나 기관연화는 적극적인 진단 과정을 하게 되면 선천성 식도폐쇄 환자에서 비교적 흔하게 발견되기 때문이다.
기관연화와 감별하여야 할 질환은 문합부 협착, 식도기관루, 심한 위식도역류 등이 있다.1-4 그러나 드물게 기관게실(tracheal diverticulum)11, 12, 선천성 식도협착(congenital esophageal stenosis)13, 그리고 선천성 윤성 연골이나 기관의 협착(congenital cricoid or tracheal stenosis)14등도 비슷한 증세를 나타낼 수 있어 주의를 요한다.
기관연화가 의심되면 식도촬영을 하여 문합부 협착이나 식도기관루의 존재여부를 먼저 확인하여야 한다. 만약 이들이 존재함이 확인되면 이를 먼저 해결하여 주는 것이 올바른 치료 순서이다. 식도촬영에서는 식도만을 확인하지 말고 투시촬영(fluroscopic study)을 통하여 기관을 채우고 있는 air column을 자세히 관찰하는 것이 좋다. 그 이유는 기관연화가 있는 경우에는 호기 시 문합부에 인접한 기관이 함몰되는 것을 투시촬영을 통하여 관찰 할 수 있는 경우가 많기 때문이다 (그림 1).
그 다음으로는 24시간 식도의 pH를 측정한다. 이는 선천성 식도폐쇄에서는 위식도역류가 비교적 흔하기 때문이다. 여러 정황이 기관연화를 강력히 시사한다면 본 예에서 시행된 것과 같이 흉부컴퓨터 단층촬영의 3차원 구성(3-D chest CT)을 시행함이 좋다고 생각한다. 그 이유는 3-D chest CT는 전신마취를 통하여야 하는 기관지경과 같이 환자에게 큰 부담을 주지 않고 손쉽게 기관연화부위를 직접 눈으로 확인 할 수 있기 때문이다 (그림 2-B). 또한 3-D chest CT를 통하여 대혈관(great vessel)의 동반기형 유무를 동시에 확인할 수 있는 장점이 있기 때문이다(그림 2-A). 본 예에서 시행한 3-D CT 영상에서는 무명동맥의 기시부가 기관의 함몰 부위와 관련되었다는 것을 확인할 수 있었다 (그림 2). 이런 정보는 대동맥고정술을 시행할 때 혈관의 고정부위와 고정방향을 결정하는 데 큰 도움이 된다. 15 또한 본 예에서와 같이 수술 후 비침습적으로 수술 효과를 확인하는 영상 방법으로도 크게 도움이 된다 (그림 2-C).
기관연화의 진단에서 기관지경은 가장 중요한 진단 수단이다. 기관연화는 결국 기관지경을 통하여 최종 확진을 내리게 된다. 소아의 기관지경 검사를 위해서는 전신마취가 필요하다. 기관연화의 진단을 위한 기관지경 검사에서는 전신마취를 하더라도 환자의 자발적 호흡을 유지한 상태에서 기관을 관찰하여야 한다. 그 이유는 기관연화에서의 기관함몰은 흉곽내 압력이 상승하는 호기에 가장 잘 볼 수 있기 때문이다. 비록 기관지경으로 확진이 이미 되었다고 하여도 기관연화의 표준 수술이라고 할 수 있는 대동맥고정술을 시행 할 때는 반드시 기관지경을 같이 시행하는 것이 좋다. 그 이유는 수술자가 기관의 함몰부의 변화를 기관지경으로 직접 관찰하면서 대동맥을 고정할 적절한 위치와 방향을 선택할 수 있기 때문이다.
앞에서 언급하였듯이 대부분 경도의 기관연화는 성장하면서 증세가 약화되고 소실되므로 특별한 치료가 반드시 필요하지 않다. 그러나 생명을 위협하는 질식 소발작이 있거나 반복적인 폐염이 있는 경우는 수술의 적응증이 된다. 특히 질식 소발작은 한 번이라도 그 증세가 있었다면 수술의 적응이 된다.
수술 방법은 현재 대동맥고정술이 가장 안전하고 성적이 좋은 방법으로 인정 받고 있다. 특히 선천성 식도폐쇄와 연관된 기관연화에서 시행된 대동맥고정술의 결과는 양호한 것으로 보고되고 있다.10, 16-17 Kiely등은 22예의 선천성 식도폐쇄와 관련이 있는 환자를 포함한 25예의 기관연화에 대동맥고정을 시행하였다.10 이중 17예(68%)는 수술 즉시 증세의 호전이 영구적으로 있었다고 보고하였으며 5예(20%)는 증세의 호전은 있었으나 폐염과 협착음(stridor)은 완전히 소실되지 않았다고 한다. 나머지 2예(12%)는 간과된 식도기관루로 인하여 증세가 오히려 악화되어 식도기관루에 대한 수술이 필요하였다고 한다. Filler등(1992)은 선천성 식도폐쇄와 동반된 기관연화 31예에서 시행한 대동맥고정술에서 27예(87%)가 효과가 있었다고 보고하였다.17 이를 그 적응증에 따라 분류하여 살펴보면 다음과 같다. 질식 소발작으로 수술 받은 21예에서는 20예(95%)가 증세가 사라졌다고 보고하고 있으며, 발관을 하지 못하여 수술을 받은 7예에서는 5예(71%)에서 즉시 발관이 가능하였다고 하며 반복적인 폐염으로 인하여 수술을 받은 3예에서는 2예(67%)에서 폐염이 반복되지 않았다고 보고하였다. 대동맥고정술은 보편적으로 좌측 제 3늑간을 이용한 접근방법을 주로 이용되고 있으며5 본 연구자 역시 이 방법을 선호하고 있다.
대동맥고정술이 이렇게
좋은 결과를 보이기는 하나 모든 환자에게서 그러한 것은 아니다. 드물기는 하나 기관연화의 부위가 상당히 긴 경우에는
대동맥고정술로는 증세가 호전되기를 기대하기는 힘들다. 이런 경우에는 연골이나 인공물질을 이용한 기관의 외부부목(external splint)을
고려하는 것이 좋다.18-20 최근에는 이러한 모든 여러 수술적 방법으로도 교정이 안 되는 경우에는 기관지경을 이용하여
Palmaz stent등을 삽입하는 방법도 개발되어 이용되고 있다 .21
결론적으로 선천성 식도폐쇄를 치료하고 있는 소아외과 의사들은 선천성 식도폐쇄와 동반되어 발생하는 기관연화에 대하여 좀 더 관심을 가지고 주도적인 역할을 하여야 한다고 생각한다.
참고문헌
1. Filler RM, Forte V: Lesion of the larynx and trachea, in O’Neill Jr. JA, Rowe MI, Grosfeld JL, Fonkalsrud EW, Coran AG (eds): Pediatric Surgery (ed 5), chap 56. St. Louis, Mosby-Year Book, 1998, Pp 865-868
2. . Filston HC, Shorter NA: Esophageal atresia and tracheoesophageal malformations, in Ashcraft KW (ed): Pediatric Surgery (ed 3), chap 27, Philadelphia, WB Saunders, 2000, Pp 362-363
3. Beasley SW: Esophageal Atresia and tracheoesophageal fistula, in Oldham KT, Colombani PM, Foglia RP (eds): Surgery of Infants and Children (ed 1), chap 61, Philadelphia, Lippincott-Raven, 1996,Pp 1026-1027
4. Benjamin B: Airway obstruction, in Freeman NV, Burge DM, Griffiths DM, Malone PSJ (eds): Surgery of the Newborn (ed 1), chap 31, New York, Churchill Livingstone, 1994, Pp 427-428
5. Kiely EM: Aortopexy, in Spitz L, Coran AG (eds): Rob & Smith’s Operative Surgery, Pediatric Surgery (ed 5), Chapman & Hall, London, 1995, Pp 132-135
6. Guy JM, Triglia JM, Louis C, Panuel M, Carcassonne M: Esophageal atresia, tracheomalacia and arterial compression: role of aortopexy. Eur J Pediatr Surg 1:261-265, 1991
7. Usui N, Kamata S. Ishikawa S, Sawai T, Okuyama H, Imura K, Okada A: Anomalies of the tracheobronchial tree in patients with esophageal atresia. J Pediatr Surg 31:258-262, 1996
8. Beasley SW, Qi BQ: Understanding tracheomalacia. J Paediatr & Child H 34:209-210, 1998
9. Blair GK, Cohen R, Filler R: Treatment of tracheomalacia: eight years’ experience. J Pediatr Surg 21:781-785, 1986
10. Kiely EM, Spitz L, Brereton R: Management of tracheomalacia by aortopexy. Pediatr Surg Int 2:13-19, 1987
11. Bhatnagar V, Lal R, Agarwala S, Mitra DK: Endoscopic treatment of tracheal diverticulum after primary repair of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 33:1323-1324, 1998
12. Danis RK: Tracheal diverticulum with recurrent apnea and segmental pulmonary atelectasis. J Pediatr Surg 17:182-183, 1982
13. Yeung CK, Spitz L, Brereton RJ, Kiely EM, Leake J: Congenital stenosis due to tracheobronchial remnant: a rare but important association with esophageal atresia. J Pediatr Surg 27:852-855, 1992
14. Han SJ, Kim, Y, Kim M, Lee K, Han A, Hwang EH: Slide cricotracheoplasty: A Novel surgical technique for congenital cricotracheal stenosis. J Pediatr Surg: 37:E36, 2002
15. Inoue K, Yanagihara J, Ono S, Kubota Y, Iwai N: Utility of helical CT for diagnosis and operative planning in tracheomalacia after repair of esophageal atresia. Eur J Pediatr Surg 8:355-357, 1998
16. Benjamin B: Tracheomalacia in infants and children. Ann Otol Rhino Laryngol 93:438-442, 1984
17. Filler RM, Messino A, Vinograd I: Severe tracheomalacia associated with esophageal atresia: result of surgical treatment. J Pediatr Surg 27:1136-1141, 1992
18. Bianchi A, Greenhough SG: Repair of long-segment tracheomalacia with free autogenous cartilage ring graft. Pediatr Surg Intern 7:236-242, 1992
19. Filler RM, Buck JR, Baboric A, Steward DJ: Treatment of segmental tracheomalacia and bronchomalacia by implantation of an airway splint. J Pediatr Surg 17:597-603, 1982
20. Vinogad I, Filler RM, Bahoric A: Long-term functional results of prosthetic airway splinting in tracheomalacia and bronchomalacia. J Pediatr Surg 22:38-41, 1987